Table of Contents
- Introduction
- History of Malaria
- Understanding Malaria: Causes and Transmission
- 3.1 The Malaria Parasite
- 3.2 Transmission Cycle
- Global and Regional Impact of Malaria
- Symptoms and Diagnosis of Malaria
- 5.1 Common Symptoms
- 5.2 Severe Malaria
- 5.3 Diagnosis Methods
- Treatment and Management of Malaria
- 6.1 Antimalarial Medications
- 6.2 Managing Severe Malaria
- 6.3 Challenges in Treatment
- Prevention and Control of Malaria
- 7.1 Preventive Measures
- 7.2 Vaccine Development
- 7.3 Public Health Initiatives
- Malaria in India: A Case Study
- 8.1 Prevalence and Statistics
- 8.2 Government Initiatives and Challenges
- Role of Dekh Bhal Healthcare in Fighting Malaria
- 9.1 Healthcare Services Offered
- 9.2 Public Awareness Campaigns
- 9.3 Collaborations and Partnerships
- Conclusion
- Call to Action
1. Introduction
Malaria is one of the oldest and deadliest diseases known to mankind. Despite significant advances in medical science, malaria remains a major global health challenge, particularly in tropical and subtropical regions. At Dekh Bhal Healthcare, we believe in empowering individuals and communities with knowledge and resources to combat this life-threatening disease. This comprehensive guide aims to provide a deep understanding of malaria, from its origins and transmission to prevention, treatment, and the role we play in fighting it.
2. History of Malaria
Malaria has plagued humanity for thousands of years, with references to the disease dating back to ancient civilizations in Greece, Rome, and China. The name “malaria” is derived from the Italian words “mala aria,” meaning “bad air,” a reflection of the ancient belief that the disease was caused by the noxious air from swamps and marshes. It wasn’t until the late 19th century that scientists discovered the true cause of malaria: the Plasmodium parasite, transmitted to humans through the bites of infected mosquitoes.
This discovery marked the beginning of modern efforts to control and eradicate malaria. Over the years, various strategies have been implemented to combat the disease, from the use of quinine in the 17th century to the development of synthetic antimalarial drugs in the 20th century. Despite these advances, malaria continues to be a significant public health issue, particularly in Africa, Asia, and South America.
3. Understanding Malaria: Causes and Transmission
3.1 The Malaria Parasite
Malaria is caused by a parasite belonging to the Plasmodium genus. There are five species of Plasmodium that infect humans, with Plasmodium falciparum and Plasmodium vivax being the most common. P. falciparum is the most deadly, responsible for the majority of malaria-related deaths worldwide.
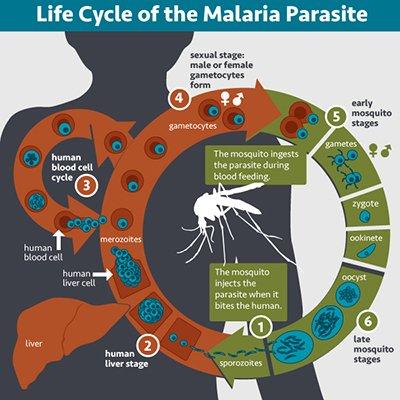
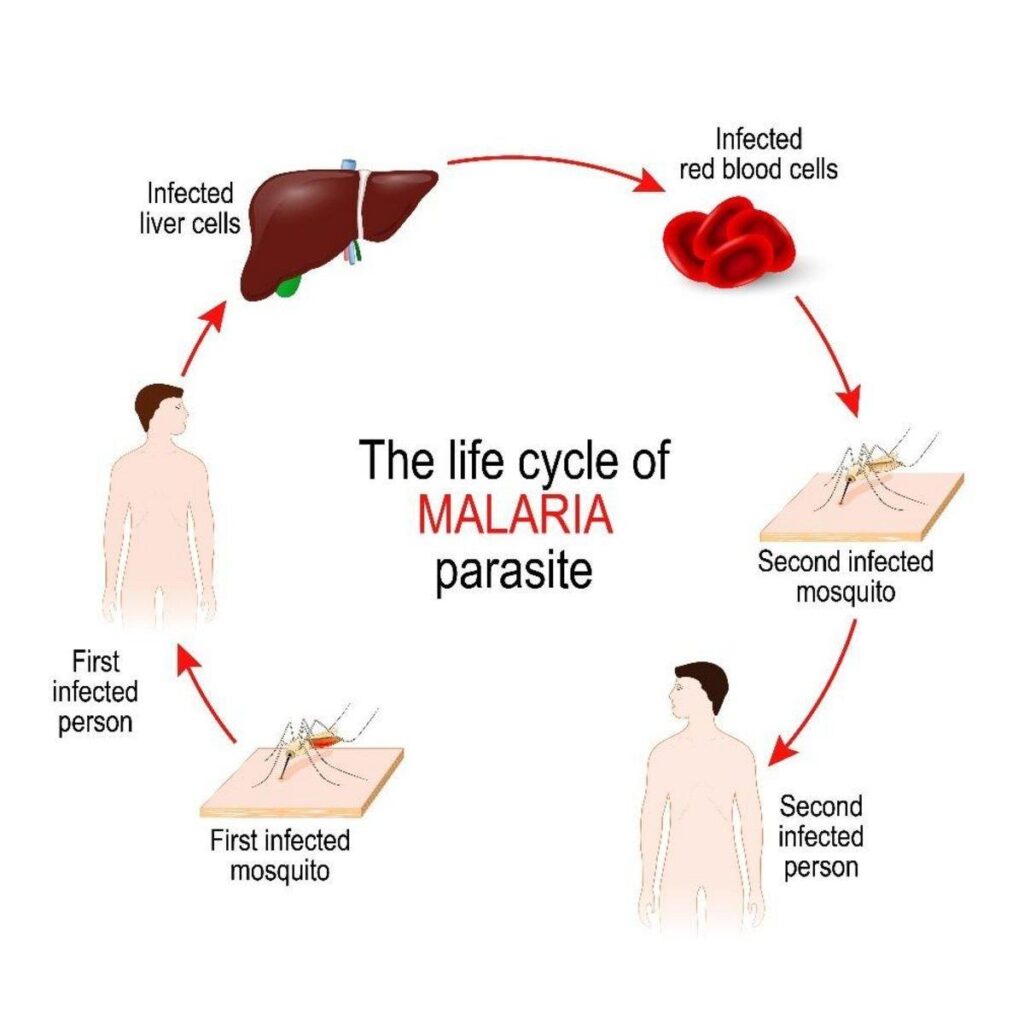
The Plasmodium parasite has a complex life cycle that involves two hosts: the female Anopheles mosquito and a human. The parasite undergoes various stages of development in both hosts, making its eradication particularly challenging.
3.2 Transmission Cycle
The transmission of malaria occurs through the bite of an infected female Anopheles mosquito. When a mosquito bites an infected person, it ingests the malaria parasites, which develop within the mosquito over a period of 10-18 days. When the mosquito bites another person, the parasites are transmitted to the new host, where they multiply and cause the symptoms of malaria.
In addition to mosquito bites, malaria can also be transmitted through blood transfusions, organ transplants, and the shared use of contaminated needles or syringes. Congenital transmission, where a mother passes the parasite to her unborn child, is also possible but less common.
4. Global and Regional Impact of Malaria
Malaria is a global health issue, with approximately 229 million cases and 409,000 deaths reported worldwide in 2019. The burden of malaria is heaviest in sub-Saharan Africa, where it is a leading cause of morbidity and mortality. Children under five years of age and pregnant women are particularly vulnerable to the disease.
In addition to its direct impact on health, malaria also has significant economic consequences. The disease reduces productivity by causing absenteeism and long-term disability, particularly in endemic regions. Malaria also places a heavy burden on healthcare systems, diverting resources away from other essential services.
Despite these challenges, significant progress has been made in the fight against malaria. Between 2000 and 2019, global malaria incidence fell by 29%, and malaria mortality rates declined by 60%. These achievements are the result of coordinated efforts by governments, international organizations, and non-governmental organizations (NGOs) to scale up malaria control interventions.
5. Symptoms and Diagnosis of Malaria
5.1 Common Symptoms
Malaria symptoms typically appear 10-15 days after an infected mosquito bite. The initial symptoms of malaria are often non-specific and can be mistaken for those of other illnesses, such as the flu. Common symptoms include:
- Fever: High fever is a hallmark of malaria and often occurs in cycles, corresponding to the parasite’s life cycle in the blood.
- Chills and Sweats: Fever is often accompanied by severe chills and profuse sweating.
- Headache: A persistent headache is another common symptom.
- Muscle and Joint Pain: Patients often experience widespread body aches.
- Nausea and Vomiting: Digestive symptoms such as nausea, vomiting, and diarrhea are also common.
- Fatigue: Severe fatigue and weakness can last for weeks or even months after the acute illness has resolved.
5.2 Severe Malaria
In some cases, malaria can progress to a severe form, particularly in young children, pregnant women, and individuals with weakened immune systems. Severe malaria is a medical emergency and can lead to complications such as:
- Cerebral Malaria: A severe form of malaria that affects the brain, leading to seizures, confusion, and coma. Cerebral malaria is often fatal if not treated promptly.
- Severe Anemia: Malaria can cause a significant reduction in red blood cells, leading to severe anemia, which can be life-threatening.
- Respiratory Distress: Severe malaria can cause fluid to accumulate in the lungs, leading to difficulty breathing.
- Kidney Failure: Malaria can cause acute kidney failure, which may require dialysis or other intensive care treatments.
- Multi-Organ Failure: In the most severe cases, malaria can cause multi-organ failure, which is often fatal.
5.3 Diagnosis Methods
Accurate and timely diagnosis is crucial for effective malaria treatment. The following diagnostic methods are commonly used:
- Microscopy: The examination of blood smears under a microscope remains the gold standard for malaria diagnosis. This method allows for the identification of the specific Plasmodium species and the level of parasitemia (the number of parasites in the blood).
- Rapid Diagnostic Tests (RDTs): RDTs are point-of-care tests that detect specific antigens produced by the malaria parasite. These tests are quick, simple, and do not require laboratory equipment, making them ideal for use in remote or resource-limited settings.
- Polymerase Chain Reaction (PCR): PCR is a molecular technique that detects the DNA of the malaria parasite. While highly accurate, PCR is more expensive and time-consuming than microscopy or RDTs, so it is typically used in research or reference laboratories.
6. Treatment and Management of Malaria
6.1 Antimalarial Medications
The primary treatment for malaria is antimalarial medications, which vary depending on the Plasmodium species, the severity of the disease, and the region where the infection was acquired. The most commonly used antimalarial drugs include:
- Chloroquine: Once the drug of choice for malaria treatment, chloroquine is now ineffective against P. falciparum in many parts of the world due to widespread resistance.
- Artemisinin-based Combination Therapies (ACTs): ACTs are the first-line treatment for uncomplicated P. falciparum malaria. These drugs combine artemisinin, a fast-acting antimalarial, with a partner drug that has a longer duration of action, reducing the risk of resistance.
- Quinine: Quinine is used to treat severe malaria and chloroquine-resistant P. vivax. It is often administered intravenously in severe cases.
- Primaquine: This drug is used to treat P. vivax and P. ovale infections, as it is effective against the liver stages of the parasite, preventing relapses.
6.2 Managing Severe Malaria
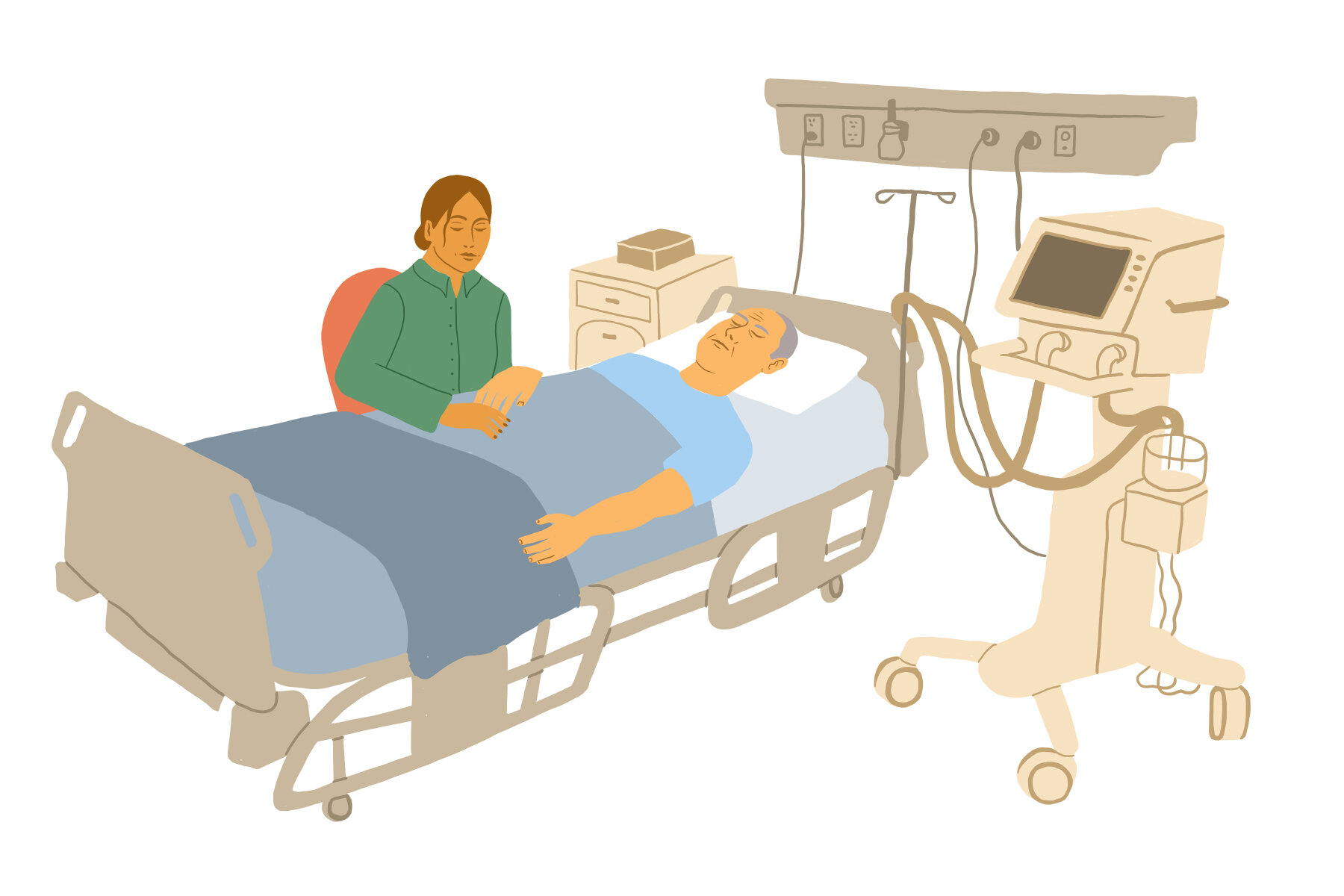
Severe malaria requires hospitalization and intensive care. Treatment involves intravenous antimalarial drugs, such as artesunate or quinine, as well as supportive care to manage complications. This may include:
- Blood Transfusions: To treat severe anemia.
- Fluid Management: To prevent or treat dehydration and shock.
- Oxygen Therapy: For patients with respiratory distress.
Dialysis: For patients with acute kidney failure.
6.3 Challenges in Treatment
While effective treatment options are available, several challenges complicate the management of malaria:
- Drug Resistance: The emergence of drug-resistant strains of Plasmodium, particularly P. falciparum, has made treatment more difficult. Resistance to chloroquine and other older antimalarials has necessitated the use of more expensive and complex therapies, such as ACTs.
- Access to Healthcare: In many malaria-endemic regions, access to healthcare facilities and diagnostic services is limited, delaying diagnosis and treatment. This can result in higher morbidity and mortality rates.
- Cost of Treatment: Although antimalarial medications are generally effective, they can be expensive, particularly in regions where poverty is widespread. This financial barrier can prevent individuals from seeking timely treatment.
- Misdiagnosis: Due to the non-specific nature of malaria symptoms, the disease is often misdiagnosed as a viral illness, leading to inappropriate treatment and prolonged illness.
7. Prevention and Control of Malaria
7.1 Preventive Measures
Preventing malaria involves a combination of vector control, personal protection, and chemoprophylaxis:
- Insecticide-Treated Nets (ITNs): Sleeping under an ITN is one of the most effective ways to prevent mosquito bites and reduce malaria transmission. ITNs are treated with insecticides that kill mosquitoes on contact, providing a double layer of protection.
- Indoor Residual Spraying (IRS): IRS involves spraying the interior walls of homes with insecticides, killing mosquitoes that rest on these surfaces. This method is particularly effective in areas with high malaria transmission.
- Use of Repellents: Personal protective measures, such as applying insect repellents and wearing long-sleeved clothing, can help reduce the risk of mosquito bites.
- Chemoprophylaxis: In some cases, travelers to malaria-endemic regions may be advised to take antimalarial medications as a preventive measure. This approach is particularly recommended for pregnant women, infants, and non-immune individuals.
7.2 Vaccine Development
The development of a malaria vaccine has been a long-standing goal in the fight against the disease. The RTS,S/AS01 vaccine, also known as Mosquirix, is the most advanced malaria vaccine to date. It provides partial protection against P. falciparum malaria in young children, who are most vulnerable to the disease. The World Health Organization (WHO) has recommended pilot implementations of the vaccine in select African countries to gather more data on its efficacy and safety in real-world settings.
While the development of an effective malaria vaccine is a significant milestone, it is not a standalone solution. The vaccine must be used in conjunction with existing malaria control measures, such as ITNs, IRS, and prompt treatment, to achieve maximum impact.
7.3 Public Health Initiatives
Global efforts to control and eliminate malaria have been spearheaded by organizations such as the WHO, the Roll Back Malaria Partnership, and the Global Fund to Fight AIDS, Tuberculosis, and Malaria. These initiatives focus on:
- Scaling Up Vector Control: Expanding the use of ITNs, IRS, and other vector control measures to reduce malaria transmission.
- Improving Access to Diagnosis and Treatment: Ensuring that all individuals at risk of malaria have access to accurate diagnosis and effective treatment.
- Strengthening Health Systems: Building the capacity of healthcare systems in malaria-endemic regions to manage and treat the disease.
- Research and Development: Supporting the development of new tools, such as vaccines, drugs, and diagnostic tests, to enhance malaria control and elimination efforts.
8. Malaria in India: A Case Study
8.1 Prevalence and Statistics
India is one of the countries most affected by malaria, with the disease being endemic in many states, particularly in the northeastern, central, and eastern regions. According to the National Vector Borne Disease Control Programme (NVBDCP), India reported approximately 3.3 million cases of malaria and around 20,000 deaths annually in the early 2000s. However, significant progress has been made in recent years, with malaria cases and deaths declining by nearly 50% between 2000 and 2019.
Despite this progress, malaria remains a public health challenge in India, particularly in remote and tribal areas where access to healthcare is limited. The disease disproportionately affects vulnerable populations, including children under five, pregnant women, and individuals living in poverty.
8.2 Government Initiatives and Challenges
The Indian government has implemented several initiatives to combat malaria, including:
- National Framework for Malaria Elimination (NFME): Launched in 2016, the NFME aims to eliminate malaria from the country by 2030. The framework outlines a phased approach to malaria elimination, with the goal of reducing malaria cases to zero in low-transmission states by 2022 and achieving nationwide elimination by 2030.
- National Vector Borne Disease Control Programme (NVBDCP): The NVBDCP is responsible for coordinating malaria control efforts across the country. The program focuses on vector control, early diagnosis and treatment, and community engagement.
- Introduction of ACTs: The government has scaled up the use of ACTs as the first-line treatment for P. falciparum malaria, replacing older drugs that have become less effective due to resistance.
However, several challenges remain in India’s fight against malaria:
- Vector Resistance: The development of resistance to insecticides used in IRS and ITNs poses a significant challenge to vector control efforts.
- Health Infrastructure: In many parts of India, particularly in rural and remote areas, healthcare infrastructure is inadequate, leading to delays in diagnosis and treatment.
- Behavioral Factors: Cultural practices, such as sleeping outdoors or reluctance to use ITNs, can hinder malaria prevention efforts.
9. Role of Dekh Bhal Healthcare in Fighting Malaria
At Dekh Bhal Healthcare, we are committed to playing a proactive role in the fight against malaria. Our comprehensive healthcare services are designed to address the needs of individuals and communities at risk of malaria, with a focus on prevention, early diagnosis, and effective treatment.
9.1 Healthcare Services Offered
We offer a range of healthcare services that are crucial in the fight against malaria:
- Malaria Screening and Diagnosis: Our team of skilled healthcare professionals provides on-site malaria screening and diagnostic services, using both microscopy and rapid diagnostic tests (RDTs).
- Treatment and Management: We ensure that all individuals diagnosed with malaria receive prompt and appropriate treatment, in line with the latest national and international guidelines. Our services include the provision of antimalarial medications and comprehensive care for severe malaria cases.
- Home Care Services: For individuals recovering from malaria, we offer home care services to ensure a smooth recovery and prevent complications. Our team of trained healthcare professionals provides personalized care and support in the comfort of the patient’s home.
9.2 Public Awareness Campaigns
Education and awareness are key components of our malaria control strategy. We conduct public awareness campaigns to educate communities about the importance of malaria prevention, early diagnosis, and treatment. Our campaigns include:
- Workshops and Seminars: We organize workshops and seminars in schools, community centers, and workplaces to raise awareness about malaria and promote preventive measures.
- Distribution of Educational Materials: We distribute brochures, posters, and other educational materials that provide information on malaria prevention and treatment.
- Community Outreach Programs: Our team conducts door-to-door visits in high-risk areas to educate individuals and families about malaria and provide them with preventive tools, such as ITNs and insect repellents.
9.3 Collaborations and Partnerships
We collaborate with government agencies, NGOs, and other healthcare providers to strengthen malaria control efforts. Our partnerships enable us to:
- Expand Access to Services: Through our collaborations, we are able to extend our services to underserved communities and reach more individuals at risk of malaria.
- Share Knowledge and Resources: We work closely with our partners to share knowledge, resources, and best practices, ensuring that our malaria control efforts are effective and sustainable.
- Support National and Regional Initiatives: We actively participate in national and regional malaria control initiatives, contributing to the overall goal of malaria elimination in India.
10. Conclusion
Malaria remains a significant public health challenge, particularly in regions where access to healthcare and preventive measures is limited. However, with continued efforts and collaboration, it is possible to control and eventually eliminate this deadly disease.
At Dekh Bhal Healthcare, we are dedicated to contributing to the fight against malaria by providing high-quality healthcare services, raising awareness, and working in partnership with other stakeholders. We believe that by empowering individuals and communities with knowledge and resources, we can make a significant impact in reducing the burden of malaria.
11. Call to Action
We encourage everyone to take an active role in preventing and controlling malaria. Whether it’s using insecticide-treated nets, seeking prompt diagnosis and treatment, or supporting public health initiatives, every action counts in the fight against malaria.
For more information on how Dekh Bhal Healthcare can assist you in malaria prevention and treatment, please visit our website at www.dekhbhalhealthcare.com.